100 Years of NLMA
The Newfoundland and Labrador Medical Association (NLMA) has played a pivotal role in shaping the healthcare landscape of the province since its inception in 1924. From its earliest days, the NLMA has been at the forefront of advocating for the interests of both medical professionals and patients, contributing significantly to the improvement of healthcare delivery, medical education, and public health initiatives throughout Newfoundland and Labrador (NL).
Through effective lobbying, strategic partnerships, and grassroots activism, the Association has influenced government policies, legislation, and funding priorities, shaping the direction of healthcare reform and innovation in the province. This review delves into the history, achievements, and ongoing contributions of the NLMA to healthcare in the province.
In the 100 years since the NLMA was founded, medical practice and healthcare generally have evolved significantly. While some issues remain constant – how to serve populations living in rural and remote areas effectively – others have emerged or changed, including disease management, technology and practice delivery options. When we consider these changes, we can see how a small group of physicians committed to a vision of healthcare changed the face of organized medicine and medical practice in Newfoundland and Labrador and laid the foundation for the active, thriving association it is today.
Looking ahead, the NLMA remains committed to its core principles of professionalism, advocacy, and service excellence, striving to build a healthcare system that is responsive, sustainable, and equitable for all residents of Newfoundland and Labrador. By harnessing the collective expertise, passion, and dedication of its members, the Association will continue to play a vital role in shaping the future of healthcare in the province and ensuring that the needs of patients and physicians are met with compassion, integrity, and excellence.
Background
Before the 1800s, doctors were rare in the colony of Newfoundland. Most of them were military or naval surgeons who treated civilians on top of their regular duties. Once restrictions on settlement were lifted, more doctors came to the colony. While their numbers increased in the 19th century, most of them were located in St. John’s. Those who settled in other parts of Newfoundland also served in other capacities, such as magistrates, teachers, and leaders in their communities.

Patients in rural and remote communities relied on doctors who travelled to see them by snowshoe, horses or boats. In Labrador, missionaries would provide limited care to those who were sick, but this was difficult given the vast distances between the communities. Hospitals were owned by the military and it wasn’t until later that the government opened civilian hospitals. The first Civic Hospital was built in 1813, the first Hospital for Mental and Nervous Disease was built in 1845 and opened in 1854 (now known as the Waterford Hospital), and another military hospital was built in 1852 on the site of the former St. John’s General Hospital.
The limited options in professional medical care contributed to the high death rates in the population of Newfoundland and Labrador. Infant mortality rates were also high and infectious diseases such as cholera, tuberculosis, smallpox and influenza spread easily. Malnutrition was a significant issue. Subsistence farming supplemented fish and game caught or hunted in season. However, the short growing season and dependence on preserved foods such as salt fish or meat contributed to this issue. Furthermore, colonization changed how Indigenous people in Labrador ate. The Moravian missionaries negatively altered traditional hunting and foraging patterns and created a dependence on European ingredients such as flour and sugar.
Legislation governing health and practice was limited. The first Board of Health and the first Public Health Act came into effect through Representative Government around 1834. At the beginning of the 20th century, a Public Health Department was established along with the appointment of the first Medical Health Officer for the Dominion. This was followed by considerable hospital construction including institutions in St. John’s, Grand Falls, Corner Brook, Grand Bank and Twillingate. Following the suspension of Responsible Government, the Commission Government set up a Department of Public Welfare, introduced a nursing service, and established the cottage hospital system in the 1930s.
The two world wars, bracketed by the global Influenza pandemic of 1918 and the Great Depression of the 1920s were a period of great social change. How people worked, where they worked, how they travelled and built families, even the political structures of Newfoundland had an impact on medicine and health.
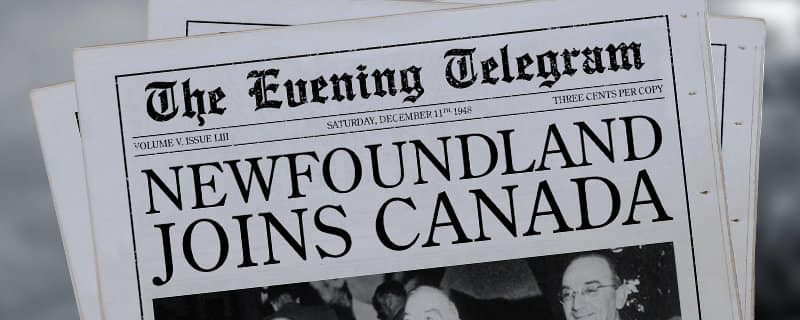
The period following Confederation in 1949 was marked by significant steps forward in health management, medical education, government infrastructure and medical technology. The improvement in economic conditions from the 1950s to the 1980s contributed to shifts in disease prevalence, personal behaviours (smoking, physical activity, and breastfeeding) and public access to healthcare through Medicare and the Provincial Medical Care Plan (MCP). The advances in computer science also led to innovations to healthcare delivery in this province, such as the Tele-Medicine Network, advances that were shepherded by physician leaders within the NLMA.
Global Pandemics in 1918 and 2020 (Sidebar)
In 2020, when the WHO declared a global pandemic due to the Corona virus (COVID-19), similarities were observed with the 1918 Spanish Flu Pandemic, which had a profound impact on Newfoundland. This deadly influenza virus, which swept across the globe in multiple and deadly waves, struck Newfoundland particularly hard, causing widespread illness, death, and social disruption. The flu resulted in multiple deaths between late fall 1918 and spring 1919.
In 1918, Newfoundland was a dominion of the British Empire, with a population that was largely rural and isolated. The Spanish Flu Pandemic reached the island, primarily through shipping routes and military personnel returning from World War I. The first cases were reported in St. John’s, the capital city, and it quickly spread to other communities across the island.
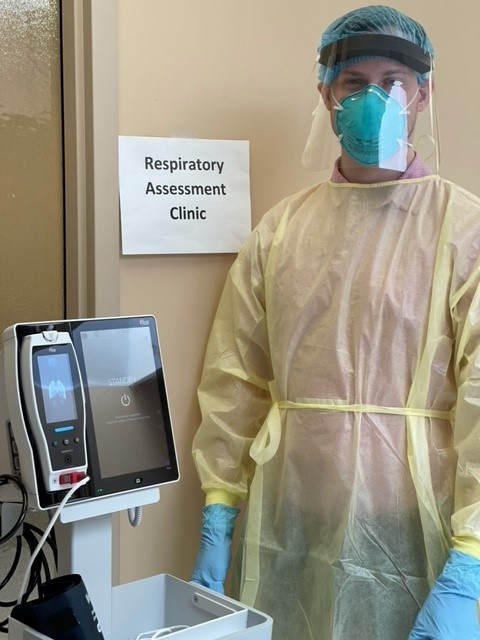
The Spanish Flu Pandemic overwhelmed Newfoundland’s limited healthcare infrastructure and resources. Hospitals and medical facilities were ill-prepared to handle the influx of patients, as there were shortages of medical supplies, personnel, and hospital beds. The rapid spread of the virus placed immense strain on healthcare workers, many of whom worked tirelessly to care for the sick despite the risks to their own health.
The impact of the Spanish Flu Pandemic was felt particularly in rural and remote communities, with some areas reporting high mortality rates due to the virus. The pandemic disrupted daily life, causing schools, businesses, and public gatherings to close, and imposing restrictions on travel and movement to prevent the spread of the disease.
One of the most tragic aspects of the Spanish Flu Pandemic in Newfoundland was its impact on vulnerable populations, including Indigenous communities and outport settlements. These communities often had limited access to healthcare services and faced additional challenges in containing the spread of the virus. As a result, they suffered disproportionately high rates of illness and death during the pandemic. Labrador was particularly affected as whole communities were devastated by the illness.
As in 1918, healthcare professionals responded swiftly and effectively to the threat of the global COVID-19 Pandemic. Led by the Chief Medical Officer of Health, Dr. Janice Fitzgerald, the province was able to limit the spread of COVID-19 through the implementation of robust public health measures. Between March 14, 2020 and April 12, 2023, there were 55,091 cases and 339 deaths confirmed in the province. The NLMA provided regular updates and supports to its members, many of whom were called into service to care for and immunize as many people as possible during the first and second waves of the pandemic.
Creating a Unified Voice
The roots of organized medicine in the colony of Newfoundland and later the province of Newfoundland and Labrador can be traced back to the early 19th century, a time of rapid social, economic, and political change in the region. As the colony grappled with the challenges of industrialization, urbanization, poverty, and disease, physicians recognized the need for a unified voice to address common concerns, advocate for professional standards, and promote the welfare of patients and practitioners alike. In 1824, six medical professionals led by William Carson[1], petitioned the governor of the colony to prevent unqualified persons from practicing medicine and securing payment for their services.
In 1867, a group of pioneering physicians came together to found the Medical Society of St. John’s led by Dr. Harry Stabb. The society served as a forum for medical education, professional networking, and collective action, fostering a sense of solidarity and shared purpose among its members. Its first goal as an organization was to establish renumeration on a fee-for-service basis. Previously, patients paid a small amount per year for all doctor calls/visits and medicines. Later renamed the Clinical Society, its purpose was to report cases and discuss medical business.
In 1896, the Responsible Government proclaimed its first Medical Act, regulating the practice of medicine through registration. The new legislation recognized not everyone was properly qualified, and one section of the Act allowed for the registration of clergy who often made half their yearly income from medical practice.
Newfoundland Medical Association is Established
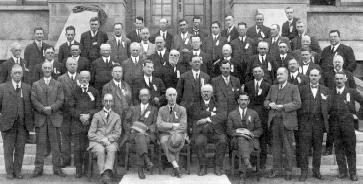
Five years after the Spanish Flu Pandemic killed hundreds and left many more ailing, doctors associated with the Clinical Society of St. John’s met with a contingent of rural physicians to investigate the expansion of the Society to become a national organization encompassing all of Newfoundland and Labrador. Drs. Arthur Anderson, Alex Forbes, and Nutting S. Fraser organized a meeting Dec 1, 1923 to which outport physicians were invited. The 34 physicians at the meeting recognized the need for closer communication and continuing medical education.
A year later, the Newfoundland Medical Association’s (NMA) constitution was formally accepted at its first convention in July 1924 with the aim of serving as a professional organization for its members and as a means to enhance healthcare. At the time, there were only about 80 doctors in active practice, for a population of approximately 265,000, with a third of those medical professionals based in St. John’s.
The original executive were President Dr. Lawrence Keegan, Vice-President Dr. Alex Forbes, and Secretary-Treasurer Dr. Cluny MacPherson.
At its first convention, the NMA established its principal tenets as follows:
- Advancement of medical science in all its branches.
- The prevention of disease with vigorous support to all health officers and health boards.
- The maintenance of a high scientific and social status of its members.
- The protection of the public against those unqualified to treat the sick or injured.[2]
The primary activities of the NMA were to represent the interests of physicians with government and to organize yearly conventions at which new information relating to medical practice was shared. In the late 1930s and early 1940s, conventions did not take place regularly due to the Depression and the Second World War.
As a country, Newfoundland had collegial relationships with other national organizations such as the Canadian Medical Association. In 1947, the NMA was invited to join the World Health Organization and the British Commonwealth Medical Conference. While the NMA still focused on conventions to bring members together, convention themes in the 1950s evolved to focus on medical economics and policy, including healthcare programs, insurance, and legislation.
The members of the NMA recognized they could not practice in isolation of political change. When Confederation was being contemplated, the NMA submitted a resume of medical services to the delegation to Ottawa regarding the Terms of Union for Confederation. After Confederation in 1949, the NMA was invited to join the CMA as a division. The NMA was restructured to fit the CMA model. Dr. Howard Drover served as the first President of the NMA in its new status as a “Division” of the Canadian Medical Association.
In 1961, the NMA’s first office was opened at the O’Mara-Martin Building in St. John’s and a part-time secretary, Mrs. Honor Carnell, was hired. In 1968, Mr. Gerry Lynch joined the NMA as the organization’s first Executive Secretary, and later, he became the first Executive Director. Mr. Lynch, who is credited with establishing many of the NMA’s processes and divisions, held the position until he was tragically killed in a car accident in 1994. He was succeeded by Mr. Bruce Squires. Mr. Squires was followed by Mr. Robert Ritter in 2001, Mr. Robert Thompson in 2013, and Ms. Gertie Mae Muise in 2024.
In 1993, the organization was renamed the Newfoundland and Labrador Medical Association (NLMA). Today, the NLMA runs its operations from NLMA House on MacDonald Drive in St. John’s with various staff representing key lines of business for the organization including contract negotiations, health policy, physician wellness, communications, advocacy and representation, and membership benefits.

Throughout the organization’s existence, it has grown steadily. In 1974, membership in the NMA became compulsory within 30 days of commencing practise as a condition of retaining a medical license. In 1991, the Association had approximately 1,000 members. As of 2024, it has more than 2500 members, which include medical students, residents, retired physicians, and about 1,500 practicing physicians.
While the mission of the NLMA has evolved, it still retains the values of the original founding members as reflected in its mandate: To represent and support a united medical profession and provide leadership in the provision of excellent healthcare in Newfoundland and Labrador. As the voice of organized medicine in Newfoundland and Labrador, the NLMA represents the political, clinical and economic interests of the province’s medical profession to its key stakeholders including governments, communities, other health professions and the public.
To represent and support a united medical profession and provide leadership in the provision of excellent healthcare in Newfoundland and Labrador.
Compensation
As the representative for physicians in contract negotiations, the NLMA today is committed to negotiating competitive compensation and benefits for members. It also advocates on behalf of all patients for a fair and equitable healthcare system in Newfoundland and Labrador.
A consistent aim of the original NMA was advocacy for improved physician compensation, working to ensure fair and equitable remuneration for medical services provided by physicians across different specialties and practice settings.
One of the first efforts at fee negotiation took place in 1938. Although individual practitioners and the Medical Society of St. John’s as a group had previously lobbied the governments of the day to address fees and rates, it wasn’t until the NMA was into its second decade as an organization that it became the voice of medical doctors in fee negotiations.
According to one account, the NMA’s first real confrontation with government dealt with the government’s proposed contract for the care of the indigent. During the 1930s, the Newfoundland treasury was depleted. The governments of the day had been reducing the amount of money allocated to medical aid. There was widespread unemployment and many people and their families lived in poverty without resources to provide shelter, heat or food.
The government offered a new contract for outport doctors. Members objected to certain terms of the contract which managed renumeration paid and conditions for doing welfare work. The NMA mobilized members and advised them to not sign the contract. NMA President Dr. Jamieson and NMA secretary Dr. Nigel Rusted met with Dr. Harris Mosdell, the Minister of Health to effect changes but they did not succeed, as all but one member signed the agreement. Nonetheless, the work undertaken by the NMA in organizing its response resulted in unifying its membership and the Association was then seen as speaking for physicians with one voice going forward.
In the late 20th and early 21st centuries, the NLMA continued its efforts in negotiating fee schedules, contract agreements, and funding models with government and health authorities. In this way, the NLMA helped to strengthen the viability and sustainability of medical practice in Newfoundland and Labrador, attracting and retaining top talent while ensuring access to high-quality care for patients.
In 2002, the NLMA took the unprecedented step of withdrawing medical service with the breakdown in government-Association negotiations. At the heart of the dispute were issues related to physician compensation and working conditions. The NLMA argued that doctors in this province were among the lowest-paid in Canada and demanded remuneration increases to bring their salaries in line with national averages. They also sought improvements in working conditions, including measures to address physician shortages and reduce administrative burdens. Amid mounting public pressure and concerns about the impact of the strike on patient care, negotiations between the NLMA and the government resumed. A tentative agreement was reached in November 2002, bringing an end to the job action. The agreement included provisions for significant pay increases for doctors, as well as measures to address some of the concerns raised by healthcare professionals regarding working conditions and physician shortages.
Since then, the NLMA has continued to negotiate on behalf of its membership and has also added its voice to influencing and guiding change with respect to the healthcare system, health policy and efforts related to the recruitment and retention of physicians.
Medicare
In pre and early Confederation Newfoundland and Labrador, medical services were the responsibility of patients. In 1867, the Medical Society of St. John’s announced at its founding meeting that doctors would be paid based on a fee-for-service basis. Over time, the Society would express its concerns regarding rates. For example, in 1880, Dr. Thomas Howley, President of the Medical Society for St. John’s, wrote to the House of Assembly protesting the reduction of vaccination fees, from 25 cents to 15 cents.
At the inaugural convention of the NMA in 1924, the NMA discussed the need for better hospital facilities, the prohibition of alcohol and the question of testing cattle for tuberculosis. It also established its first fee schedule: $1.00 for a visit, $15.00 for midwifery, $20.00 for treatment of a simple arm or leg fracture, and $50.00 for a laparotomy. In 1929, the NMA protested the reduction in the mileage fee for outport travel – from $1 to 25 cents – for what was then termed pauper cases.
In 1934, Dr. John Olds in Twillingate devised a system called the Blanket Contract, which was in fact the approach used in the early 1800s. He realized very quickly in his tenure as the superintendent of the hospital that goods such as fish or potatoes solely provided in exchange for medical treatment or doctor’s visits could not pay salaries or buy equipment. This contract cost 44 cents a year per person and provided them with full medical service.
The establishment of the cottage hospital system by the Commission Government in 1934 formalized the Blanket Contract. Families and individuals were listed on the hospital rolls as subscribers, indicating they had paid a fee for future treatment. The fee was $10 per family or $5 per person, per year. Later the fee increased to $15 per family and $7.50 per person. In communities equipped only with nursing stations, the fees were $6 for families and $3 for individuals.
With Confederation, Newfoundland was able to participate in federal initiatives regarding medical care coverage. In 1955, Dr. Leonard Miller, a former NMA president (1942), led the development of initiatives to increase children’s access to medical care by covering physician fees. In 1957, the province joined the Children’s Hospital Plan followed by free Hospital Medical Care. The province also joined the Federal-Provincial Hospital Insurance Program in 1958. Between 1958 and 1966, the members of the NMA contributed time to committees and meetings to get MCP running in cooperation with Medicare. In 1968, in anticipation of the enactment of the federal legislation, the NMA established a comprehensive fee schedule as a guide to dealing with insurance claims and third-party compensation. In 1969, on April 1, the Canadian Medical Insurance Act came into effect.
Medical Education
The NLMA has played a central role in supporting the professional development and continuing education of physicians throughout their careers. Through conferences, workshops, seminars, and online resources, the Association has offered opportunities for physicians to enhance their clinical skills, stay abreast of emerging medical trends and technologies, and engage in lifelong learning to provide the best possible care for their patients.
The establishment of the School of Medicine at Memorial University (MUN) in St. John’s marked a significant milestone in the province’s efforts to address its healthcare needs and develop a sustainable healthcare workforce. Prior to the establishment of the medical school, Newfoundland and Labrador faced significant challenges in recruiting and retaining physicians, particularly in rural and remote areas.


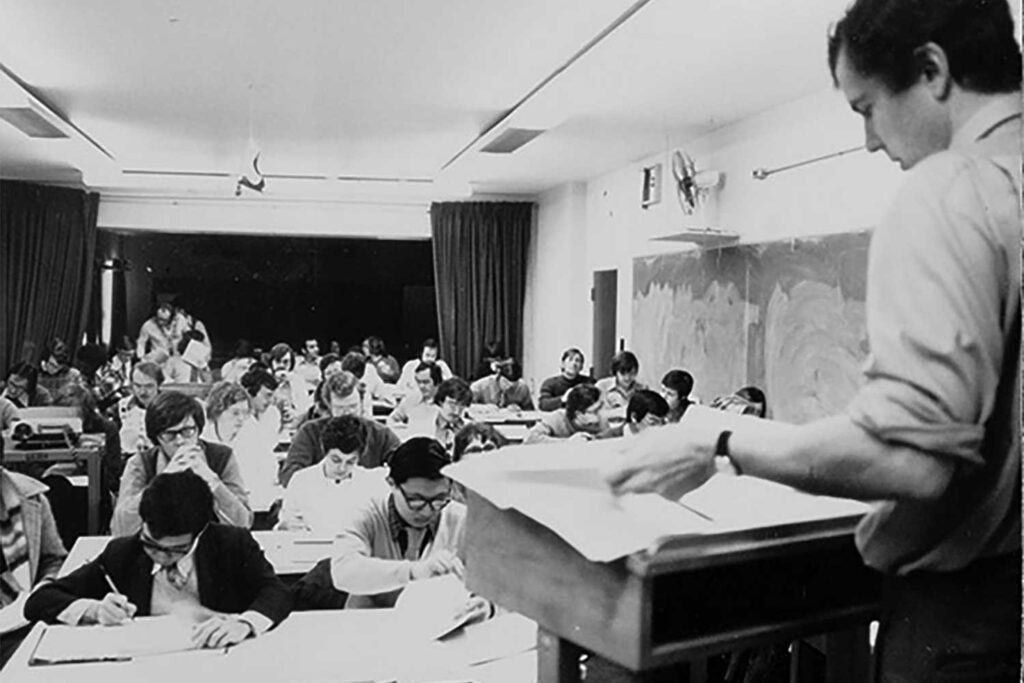
The limited availability of medical education and training opportunities within the province meant that many aspiring physicians had to pursue their education elsewhere, often leading to a “brain drain” as talented medical professionals left the province to seek opportunities elsewhere. Before the medical school was opened in 1967, the medical profession relied on the NMA’s annual conventions to support continuing medical education, as well as travelling for other continuing medical education opportunities.
Recognizing the need to address these challenges and develop a local supply of healthcare professionals, the NMA was heavily involved in advocacy for the creation of the province’s medical school. In 1958, Dr. Ron V. Christie, Chairman of the Department of Medicine at McGill University, proposed the idea for a medical school in Newfoundland to the Deputy Minister of Health, Dr. Leonard A. Miller, after speaking at a Newfoundland refresher course for family physicians. In 1961, MUN raised the question of establishing a medical school.
To ensure Newfoundland was chosen as a site for the new medical school, the NMA established a Committee on Medical Education to lead the advocacy campaign. In 1962, the NMA submitted a brief to the Hall Royal Commission on Health, recommending that a Newfoundland Medical School be established. The NMA argued that a locally-based medical school would not only help address the province’s physician shortage but also contribute to the overall health and well-being of Newfoundland and Labrador residents by ensuring access to high-quality medical care. Later in 1962, the Hall Royal Commission on Health Services released its findings related to Newfoundland’s medical health services. It recommended four or five new medical schools for Canada, one of which might be in the Atlantic Provinces.
In 1964, Dr. Ian Rusted summarized the key arguments in support for a medical school in the province, calling it “highly desirable.” In 1966, the NMA submitted a second brief to the Royal Commission on Health, which later recommended Newfoundland as one of the preferred sites for a new medical school. A year later, following joint efforts between the provincial government, the NMA and the university, Premier Joesph Smallwood announced the provincial government’s support for the establishment of a medical school at MUN. According to the Medical School Archives, the Evening Telegram reported on Feb. 1, 1967 that “the Brain Commission recommended that a teaching hospital of at least 400 beds – equal in size to the Grace General Hospital – be established at Memorial University and that such a hospital, in conjunction with a medical school capable of receiving 40 students annually, be built on the campus as soon as possible.”
In 1969, MUN formally opened the Faculty of Medicine and Dr. Ian Rusted was named the first Dean of Medicine. The first group of students (16) were admitted in September 1969 and another 32 students were admitted in 1970. In 1971, 33 Newfoundlanders were accepted for study at the MUN Medical School. In the same year, 22 students were conferred the degree of Bachelor of Medical Science for the first time at MUN.
The creation of the medical school at MUN represented a significant investment in the province’s healthcare infrastructure and human capital, providing aspiring physicians with the opportunity to receive medical education and training within Newfoundland and Labrador. A number of members of NMA comprised the membership of the school’s initial faculty and onwards including leadership as Deans and senior professors at the School of Medicine.
Public Advocacy
The NLMA has long recognized the importance of community engagement and public outreach in promoting health and wellness and addressing the social determinants of health that impact the well-being of individuals and communities. Through initiatives such as public health campaigns, health education programs, and community partnerships, the Association has raised awareness of health issues, promoted preventive measures, and empowered individuals to take control of their health and make informed decisions about their care.
Following the founding of the NMA, the organization took seriously its goal of supporting public health initiatives. Early issues addressed by the NMA included patient care, immunization, hospital conditions, and school health. The organization’s members and its committees made recommendations on the Public Health Act, addressed the purity of local milk supplies, and supported changes in the Customs Act regarding medical supplies, among many other issues.
Between 1940 and 1945, the NMA appointed a special Nutrition Committee to help with a Canadian Medical Association study. In 1945, the Canadian Medical Association Journal (CMAJ) published the results of its nutrition survey, in which the study authors reported on the high infant mortality rate (almost twice as high as that of Canada) and the high death rate from tuberculosis (almost three and a half times the rate of Canada’s). Both were linked to poor nutrition and also to the general fitness of the population.
The CMAJ study concluded, “The poor nutritional status of the people of Newfoundland may well be in large part responsible for their impaired health and efficiency.” Members of the NMA supported the work of the research team. These were Dr. James McGrath and Dr. Robert Dove, Chairman and Secretary respectively of the Nutrition Council of the NMA. As well, Dr. McGrath, Dr. Dove and Dr. Miller assisted in various aspects of the survey.
The 1945 study was controversial, especially for suggesting that the citizens were responsible for their own poor health. When the survey was repeated four years later, conditions had improved significantly. The Newfoundland government had acted on the NMA’s Nutrition Council recommendation to fortify imported flour, in part to avoid comparisons with the distribution of whole wheat “dole” flour during the Depression years. The Second World War brought greater prosperity, the population had increased, Newfoundland’s status had improved strategically on the global front, and the health status of the population had improved. The NMA continued its efforts with respect to increased attention to nutrition in later years. These days, the NLMA has partnered with other like-minded groups to support multiple public education campaigns.

The NLMA has continued its work with public health advocacy by partnering with other organizations such as the NL Public Health Association, the Association of Registered Nurses NL (now the College of Nurses NL), the Canadian Cancer Society NL, Kids in Safe Seats, the Heart and Stroke Foundation NL, the Lunch Association of NL, the Alliance for the Control of Tobacco among others, to work collaboratively to effect change on important public health issues.
The organization has collaborated on issues related to smoking tobacco, smoking cessation, second hand smoke in the workplace and more recently cannabis use and vaping.
NLMA leadership has also supported research and public education regarding child health safety including infant car seats, bicycle helmets, and All-Terrain-Vehicle (ATV) use. In 2005, it conducted research on bicycle helmet safety and successfully lobbied for the implementation of bicycle helmet regulation in NL.
In 2010, the NLMA presented research and recommendations supporting the need for a fully-resourced comprehensive model of care that reflects the full continuum of health and community services. In 2011, the NLMA sponsored a Seniors Summit to develop policy recommendations for the medical treatment of the province’s seniors. The Seniors Summit focused specifically on the medical model of healthcare delivery in the community and the acute care system. Physicians, nurses and social workers collaborated to identify elements of a new medical model which would successfully address the issues and barriers experienced at the frontline service level in hospitals, nursing homes and in the community.
In 2016, pre-Health Accord NL, the NLMA launched consultations with physicians and patients on building a safe and sustainable healthcare system in response to the provincial government’s multi-year renewal initiative to find savings in the provincial budget. This resulted in recommendations and action plans in the areas of utilization management; role delineation of facilities; the expanded use of technology; end of life care; coordination of services; and, accountability. It was followed by the release of findings from the NLMA’s 2017 provincial Forum to Determine the Need for a Review of Health Facilities and Services in Newfoundland and Labrador, which included input from more than 130 health system stakeholders. The findings formed the basis for the NLMA’s proposal to government entitled Rebuilding NL Health, which provided specific suggestions on the scope and processes for a review of health facilities and services. The provincial government went on to develop Health Accord NL, which included input from the NLMA and physicians.
In 2018, the NLMA partnered with the Newfoundland and Labrador Chapter of the College of Family Physicians of Canada and Memorial University’s Discipline of Family Medicine to release the joint report Family Medicine in Newfoundland and Labrador: A Ten-Year Vision. The paper described the forces creating problems in the healthcare system, the strategies that are working well, and the steps needed for moving family medicine forward. The paper served as the basis for a Shared Agenda on Family Medicine between the NLMA and the provincial government, which included joint priorities and commitments. In 2019, the NLMA released a Family Physician Human Resource Forecast identifying the projected demand for physicians over the next 10 years to meet the needs of the population and provided recommendations for a health human resource plan.
Just before the COVID-19 pandemic, the NLMA held a Virtual Care Summit to explore how virtual care technologies would transform the landscape of healthcare in the province. Recommendations produced following the summit would prove valuable as the province’s healthcare system was about to drastically shift to using virtual services during the public health emergency. The NLMA would later launch a campaign to increase COVID-19 vaccine uptake and produced recommendations for the provincial government on re-opening medical services following the initial shutdown.
The Association also speaks to the media and releases recommendations on key issues facing physicians, patients and the healthcare system. In recent years, the NLMA has put forward recommendations for health system sustainability, fixing the crisis in rural health centres, addressing surgical cancellations and backlogs, primary care reform among other issues.









System Change
In looking at the NLMA’s 100 years of service in this province, system change has been a key focus in supporting long term improvements in healthcare for the people of Newfoundland and Labrador. From individual practice work to hospital care, Newfoundland and Labrador’s physicians have been engaged in system reform since the early 1800s.

Three key physicians who helped change the face of healthcare and medical practice were Dr. William Carson, Dr. Harry Stabb, and Sir Wilfred Grenfell. Carson initiated the first medical society in St. John’s and undertook to effect significant reforms to healthcare delivery in the early part of the 19th century. Dr. Stabb founded the Medical Society of St. John’s in 1867. He was also a leading proponent for the provision of medical services to people with mental illness. Grenfell led the development and delivery of organized health services in Northern Newfoundland and Labrador in the late 19th and early 20th centuries, and the International Grenfell Association continued to provide services in Northern Newfoundland and Labrador until the 1990s.
Development of Cottage Hospitals

The period between the First and Second World Wars was one of economic deprivation as various governments struggled to cope with the extreme poverty faced by the people in Newfoundland and Labrador. Despite the conversion of military hospitals to civilian units in the 1920s and 1930s and the addition of hospitals in Northern Newfoundland and Labrador as a result of the Grenfell Association, there were only 12 hospitals for the island, and six of those were in St. John’s. They were almost always filled to capacity and their conditions were a continuing concern of the NMA.
On its appointment in 1934, the newly formed Commission of Government moved swiftly to take action on the recommendations contained in the 1930 report of the Royal Commission on Health and Public Charities. The result was an expansion of hospitals and nursing stations in underserved areas of the country, almost all outside of St. Johns. Between 1935 and 1954, 19 cottage hospitals were established in Newfoundland while the Grenfell Association operated hospitals and nursing stations in Northern Newfoundland and Labrador.
Cottage hospitals were typically small facilities staffed by a limited number of healthcare professionals, including nurses, family physicians, and sometimes specialists on rotation. While they lacked the comprehensive services and resources of larger urban hospitals, they provided essential medical care, including basic diagnostic services, maternity care, minor surgeries, and emergency treatment.
The first cottage hospital was built in Argentia in 1936 and the last was built 30 years later in 1966 on Bell Island. The cottage hospital system had its supporters and detractors. According to Dr. Leonard Miller, past president of the NMA (1942) the cottage hospital initiative could be seen “as a far-sighted excursion into socialized medicine to a bureaucratic perversion of medical practice.” Nonetheless, in his review of the cottage hospital system for the NMA newsletter in 1974, Dr. Miller noted there were conflicts between the government and physicians regarding the matter of fees and compensable services. He suggested that greater attention to benefits and engagement in the system’s development would have led to greater levels of satisfaction among the physicians affiliated with the cottage hospitals.
Hospital ships

The hospital ships played a vital role in delivering healthcare services to areas with limited access to medical clinics or hospitals. Many coastal communities lacked permanent healthcare facilities, making it difficult for residents to access medical care, particularly in emergencies or during harsh winter months when travel by land or sea was treacherous.
In 1935, The M/V Lady Anderson (right) was the first vessel used as a clinic boat in the Cottage Hospital system. Dr. Nigel Rusted, a Newfoundlander, was the first physician to serve on the clinic boat, which was used to bring medical services to patients in remote communities.
The hospital ships operated on regular schedules, visiting designated ports and harbours along the coast of Newfoundland and Labrador. They served as floating clinics, providing medical consultations, diagnostic tests, and treatments to residents who might otherwise have gone without care. In addition to delivering medical services, the hospital ships also served as centres for health education and promotion, raising awareness about preventive measures and healthy living practices.



Over time, advances in transportation and healthcare infrastructure led to changes in the way medical services were delivered in Newfoundland and Labrador. As road networks improved and permanent healthcare facilities were established in more communities, the need for hospital ships diminished. The last of the Newfoundland Hospital Ships, the MV Lady Hope, was decommissioned in 1966, marking the end of an era in maritime healthcare delivery in the province.
Child Health & Janeway Children’s Hospital

In 1957, pediatrician Dr. Clifton Joy chaired an NMA study group to look at the province’s needs with respect to child health. The group concluded existing facilities were inadequate and recommended the government build a new hospital in St. John’s.
An NMA committee headed by Dr. Ted Shapter in 1961 was set up to study possible uses for a decommissioned military hospital in Pleasantville (Fort Pepperell). A children’s rehabilitation centre was also under consideration given the numbers of children affected by two polio epidemics in the 1950s.
Dr. Joy continued to advocate for the children’s hospital including running for elected office as MHA to advance his cause with the provincial government. Following an increase in cases of scurvy in 1963, along with a serious outbreak of gastroenteritis that resulted in the deaths of more than 100 infants, greater public and political attention focused on children’s health generally. The report of an external investigation into the infantile gastroenteritis outbreak recommended the establishment of a child health centre in the capital. The recommendation for a children’s hospital was also supported by the Brain Report (Royal Commission on Health).
In spring 1966, following the Premier’s decision to approve the former military hospital as a children’s health centre almost two years previously, the NMA submitted another report to the Minister of Health indicating its approval for the decision. The Janeway Child Health Centre opened August 9, 1966.
Healthcare System Reform
In recent years, the NLMA has been actively engaged in efforts to reform the province’s healthcare system, advocating for a more integrated and patient-centered approach to care delivery that emphasizes collaboration, continuity, and accountability. By promoting team-based care models, electronic health records, and quality improvement initiatives, the Association aims to optimize health outcomes, improve patient satisfaction, and achieve greater value for healthcare investments.
As a trusted voice in healthcare policy and reform, the NLMA provides expert input and guidance on a wide range of issues affecting the delivery, organization, and financing of healthcare services in Newfoundland and Labrador. By conducting research, publishing reports, and collaborating with stakeholders, the Association helps to inform evidence-based decision-making and shapes the development of health policies and programs that address the evolving needs of the population.
The NLMA’s policy priorities encompass a broad spectrum of healthcare issues, including access to care, patient safety, health equity, and physician well-being. By advocating for investments in primary care, mental health services, and chronic disease management, the Association seeks to enhance the accessibility and effectiveness of healthcare services, particularly in underserved and remote communities where disparities in health outcomes persist.
In the past three decades, the NLMA has examined primary care, family practice renewal and health system restructuring. In 2016, the NLMA and the provincial government achieved a funding agreement which would allow the Association to establish a Family Practice Renewal Program dedicated to primary healthcare renewal. The three core objectives included establishing family practice networks, enhancing the fee-for-service schedule through a Fee Code program, and supporting practice improvement.

In 2021, the NLMA commissioned an extensive consultation process with physicians to determine their perceptions of the Health Accord’s proposed framework for healthcare system redesign. The Health Accord’s final report identifies strategic directions for rebalancing the health system and addressing social, economic, and environmental factors that impact health. The NLMA provided information guidance and feedback to the Health Accord’s committees on a regular basis to share the views and priorities of physicians.
The chairs of the Health Accord recommended the task force be transformed into a stakeholder advisory council that would include representation from the NLMA and other stakeholders for high-level strategic consultation. As a result of its consultations with members, the NLMA continues to monitor the creation of community care teams and the development of the blended capitation model for family medicine within the team-based approach to care within the NL Health Services structure.
Innovations, Challenges and Opportunities
Despite its many achievements, the NLMA faces a number of challenges in fulfilling its mission to advance the interests of physicians and improve healthcare in Newfoundland and Labrador. The province’s geographical vastness, sparse population, and aging demographics with a high disease burden present unique challenges in delivering equitable and accessible medical services, particularly in rural and remote areas where physician shortages and infrastructure deficiencies continue to persist.
The NLMA has been vocal in the media regarding the plight of rural health centres which is one component of the broader family physician shortage. The Association’s advocacy is also responsible for the introduction of eDOCSNL, the provincial Electronic Medical Record (EMR). The EMR is integrated with other provincial information systems providing access to such health information as demographics, medical and drug history, laboratory results and diagnostic imaging. It also linked to MCP and HEALTHe NL the provincial health record.
Even before the pandemic of 2020-2024 was on the horizon, the Association had been deeply involved with issues relating to virtual care. In 2019, the Association released its Virtual Care Strategy, the result of a collaborative process with physicians and other stakeholders. The NLMA’s virtual care strategy focused primarily on services offered through integrated video, voice, instant messaging and email, augmented by remote patient monitoring and connected information and decision support systems. The strategy recognized that virtual care will play a large role in the services provided by many other healthcare providers and teams of providers.
Gender Equity (Sidebar)

While the first seven decades of the Association were dominated by men, the Association has supported women as leaders in the NLMA. In 1991, the Association elected its first female president, Dr. Faith Stratton. Ten years later, in 2001, the Association elected its second female president, Dr. Lydia Hatcher. Between 2003 and 2021, the Association was led by ten other female physicians, including a five-year stretch from 2017 to 2021 when all the NLMA presidents were women.
The numbers of women studying medicine in Newfoundland and Labrador and across the country has steadily increased: In 1958, 5.3% of the medical degree graduates in Canada were female; 10.9% in 1968; 29.2% in 1978, and 35.6% in 1982 (MUN Medical School Archive). In 1982, more than half of the 57 students registered at the MUN Faculty of Medicine (Class of 1986) were women, the first time the number of women surpassed the number of men.
Today (2024), 44% of all practicing physicians in the province are female.
Today (2024), 44% of all practicing physicians in the province are female.
In 2022, the NLMA issued a white paper, Mind the Gap: Addressing Gender Equity in Physician Compensation, Newfoundland and Labrador. The discussion paper documented existing gender-based inequities in physician compensation and outlined a series of potential solutions and approaches to mitigating them. The committee which spearheaded the development of the white paper consulted with the NLMA membership and also examined other Canadian and international research. The report’s findings have ensured that a gender lens is applied to all future NLMA contract negotiations with the provincial government.
Leadership
The leadership of the NLMA has been comprised of elected leaders who accept responsibility for the organization’s governance and general members who guide and influence change and innovation in the delivery of healthcare in Newfoundland and Labrador. Not all of their many contributions in the past 100 years have been documented; however, their influence is evident in the Association’s success as a voice for organized medicine and as leaders in medical policy.
In his final address to the membership before retiring as the Association’s first president. Dr. Keegan said:
We are the Custodians of the people, where the great questions of public health and medical institutions are concerned, and it is up to us to assert ourselves to offer our advice and our influence to improve health conditions all over the island. There cannot be happiness without health and there cannot be health without hygienic surroundings nor can there be prosperity and we all want to see Newfoundland healthy and prosperous. She is a great country to live in. She has the healthiest climate in the world and although medical men may have better facilities and easier times in other parts, there is a fascination about this old spot that captivates and holds one.
- There have been 98 presidents since the organization was founded in 1923 and formally recognized in 1924.
- Three physicians served two terms as President: Dr. L. Keegan (1923 and 1924), Dr. Cluny MacPherson (1933 and 1934) and Dr. D. Cant (1957 and 1965).
- Four presidents of the Association served as Ministers of Health in the provincial government: Dr. J.M McGrath (1944), Dr. Hugh Twomey (1961), Dr. T. Rowe (1967) and Dr. John Haggie (2002).
- Two sets of presidents have family connections: Dr. Harry Roberts (1950) was the father of Dr. Peter J. Roberts (1993) while Dr. Andrew Major (2004) and Dr. Stephen Major (2024) are brothers.
- There have been 12 women who served as presidents: Dr. Faith Stratton (1991), Dr. Lydia Hatcher (2001), Dr. Susan King (2003), Dr. Terry O’Grady (2006), Dr. Elizabeth Callahan (2008), Dr. Sandra Luscombe (2011), Dr. Wendy Graham (2014), Dr. Lynne Dwyer (2017), Dr. Tracey Bridger (2018), Dr. Charlene Fitzgerald (2019), Dr. Lynette Powell (2020), and Dr. Susan MacDonald (2021).
- Dr. Cluny MacPherson (1933 and 1934) is the inventor of the gas mask and also served as a president of the St. John’s Clinical Society (pre-cursor to NMA) and the Registrar of the Newfoundland Medical Board.
- The first Newfoundland-born president is most likely Dr. C. A. Forbes (1925) of Bonavista.
- Dr. Leonard Miller (1942) was instrumental in many key initiatives in Newfoundland’s medical services, including the cottage hospital system (1934), the children’s health plan (1955), Medicare (1966) and the medical school (1969) at Memorial University.
- Dr. John Olds (1943) is credited with the re-invention of medical insurance, which he called the Blanket Contract. It was later implemented throughout the cottage hospital system before Medicare was developed in Canada.
- Dr. James McGrath (1944) served as an Assistant Deputy Minister of Health 1943 to 1956 and was later elected as an MHA in 1956. He served as Minister of Health and Minister of Finance.
- Before serving as NMA president Dr. Harry Roberts (1950) served as Honorary Secretary from 1939 to 1947. He was the first Newfoundlander to serve as President of the Canadian Medical Association (CMA) in 1971.
- Dr. Francis O’Dea (1960) set up the first specialty in Obstetrics and Gynecology and co-authored with Dr. Hatcher (University of Toronto) the Survey of Maternal and Child Health for the Newfoundland Department of Health.
- Dr. Hugh Twomey (1961) was elected as an MHA in 1976 and served as Minister of Health and Minister of Public Works and Services.
- Dr. Alvin Mercer (1966) was the province’s first urologist and the last doctor in the province to sign up for Medicare. He later worked in the MCP audit division.
- Dr. Frank Duff (1972) initiated a program in co-operation with the Department of Health to recruit a team of doctors to provide essential medical services to the Labrador West Hospital during a critical shortage of medical services in this region. He led by example by being one of the first to volunteer.
- Dr. Peter Roberts (1990) was the fifth and last director of the International Grenfell Association. His father was also past president of the NMA in 1950.
- Dr. Norman Lush (1993) was considered the father of neurology in Newfoundland and Labrador. He was a founding member of both Wheelchair Sport and the Hub.
- Dr. Gerard Farrell (2023) developed the province’s first online chemotherapy order entry system used in patient care.
[1] Image of William Carson, https://www.heritage.nf.ca/articles/society/19th-century-health.php
[2] Dr. David Parsons, NLMA Newsletter, pp 23-26, Vol. 16, No. 3, 1974.
Various Photos provided by Early Days of the Medical School virtual exhibit (including COLL-041 Telemedicine and COLL-007 HSIMS Photograph Collection), Faculty of Medicine Founders’ Archive, Health Sciences Library, Memorial University.
